Table of Contents:
- What Exactly is Bariatric Surgery?
- Bariatric Surgery Benefits
- Which Procedure is Best?
- Your New Diet
- The Emotional Rollercoaster
- Does Insurance Cover Bariatric Surgery?
- How Do I Get Started?
- The 10 Commandments for Bariatric Success
- Conclusion
What is Bariatric Surgery?
Commonly referred to as weight loss surgery, bariatric surgery is one of the few weight loss treatments that have a history of proven results. The term bariatric surgery refers to any surgical procedure on the stomach or intestines to induce weight loss.
Bariatric surgery is a term that encompasses several procedures. The most common procedure in the United States is gastric sleeve surgery (sleeve gastrectomy). Gastric bypass is the second most often performed bariatric surgery and Lap Band surgery is the third most popular procedure in the United States. Duodenal Switch is another very effective, although less frequently performed, procedure.
Newly FDA approved procedures such as gastric balloons fall under the bariatric surgery umbrella as well.
Bariatric Surgery Benefits: What You Can Expect
Let’s start by taking a look at what you can expect from bariatric surgery.
On top of decreasing medications and losing weight, bariatric surgery has other benefits as well.
- Reduced risk of cancer – SOARD: Bariatric surgery reduces cancer risk in morbidly obese patients
- Improved self-esteem and quality of life – International Journal of Obesity: Does obesity surgery improve psychosocial functioning? A systematic review
- Improvement in fertility and complications during pregnancy – Human Reproduction Update: Reproductive outcome after bariatric surgery: a critical review
- Longer life – The New England Journal of Medicine: Long-term Mortality After Gastric Bypass
Improved Comorbidities
Below is a list of common comorbidities that may be improved with bariatric surgery.
- Arthritis
- Sleep Apnea
- High Blood Pressure
- High Cholesterol
- Type 2 Diabetes
- Venous Stasis Disease (Collection of Blood in the Lower Limbs)
- Soft Tissue Infections
Type 2 Diabetes is extremely common in morbidly obese patients. Data shows that laparoscopic gastric bypass, lap gastric banding and gastric sleeve surgery can reduce your dependence on medication and often completely resolve the condition.
Less frequent comorbidities that are occasionally accepted by insurance include:
- Congestive Heart Failure
- Fatty Liver Syndrome
- Gall Bladder Disease
- Depression
- Stroke or Stroke Risk
- Inability to Carry Out Daily Activities
- Psychosocial Stress Resulting From Obesity
- GERD (Acid Reflux Disease)
- Gout
- Knee and back pain
- Migraines
Non-Scale Victories
Bariatric surgery is not a cosmetic procedure. You will lose weight and may look better. But the success of bariatric surgery should be based on a reduction of co-morbidities, improved longevity, and an improved quality of life, not numbers on a scale. Are you happier, healthier, and going to live longer?
Let’s take a look at some non-scale victories.
- When you don’t need the extender belt on an airplane.
- When you can shave your legs without a struggle or mirror.
- When you make it up the stairs without breaking a sweat.
- When you are not embarrassed to take a picture.
- When you get to wear that dress that you’ve had in your closet for years.
- When you can cross your legs.
- When you aren’t the biggest person in the room.
- When you fit comfortably in a seat.
- When you can wrap a standard bath towel around your body.
- When you don’t have to shop at plus size stores.
- When you can get in and out of booths easily at restaurants.
- When your joints don’t hurt at the end of the day.
- When you are not the ‘fat’ member of your group of friends.
The list can go on and will be different for everyone. Losing weight does so much more than just improving medical conditions and lowering the number on your scale.
But you have to stay focused, and you have to change.
Celebrate your non-scale victories. Make a list of the things you want to do that your weight has prevented you from doing and reward yourself when you reach those goals. Don’t reward yourself with food. A manicure, tickets to a concert or sporting event, a night out with the friends are great rewards.
A Brief History of Bariatric Surgery
In the 1950s, weight loss surgery began with the intestinal bypass. This surgical procedure shortened the length of the small intestine. The intestines absorb calories and macronutrients. And if this area were shorter, then there would be less absorption of calories and macronutrients as the food worked its way out of the patient’s body.
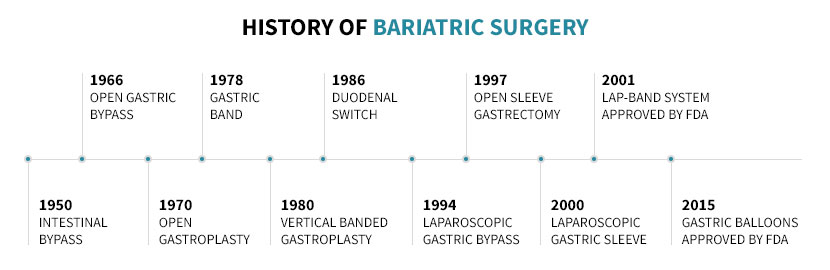
In 1966, Chikashi Ito and Dr. Edward E. Mason developed gastric bypass surgery. In the procedure, the stomach was resected, and a smaller portion of intestines was bypassed. With a smaller stomach, patients found it harder to eat large meals, and the bypassed intestines led to less calorie absorption. The result? Weight loss.
Because of these groundbreaking developments, Mason is now commonly referred to as being the “father of obesity surgery.”
Most bariatric surgery procedures are now performed laparoscopically. Laparoscopic surgery is also called “minimally invasive surgery.” Three to six small incisions are made. Then 5 to 15mm instruments and a camera are inserted into the patient’s body. Recovery is quicker, and patients experience less pain.
Learn more about the history of bariatric surgery.
So Which Procedure is Best?
Looking at the timeline above, you’d think that gastric balloon surgery is the latest and greatest procedure for weight loss. Or you may think that the Lap Band is the best because you’ve heard so much about it.
Everyone has a different relationship with food, different medical histories, and different lifestyles. One procedure does not fit all.
Open and honest conversations with your bariatric surgeon will help you choose the procedure that best fits your personality, level of risk aversion, and lifestyle.
Feel free to take our Bariatric Surgery Selector Test, but again, open and honest conversations with your bariatric surgeon will lead to the best procedure for you.
Key Points:
- Not all bariatric surgeons perform every procedure.
- There could be a strong bias towards gastric banding if your surgeon only performs the Lap Band procedure.
- Ask your bariatric surgeon which procedures he or she performs, and if he/she doesn’t perform a procedure, ask why.
- The support and education from the bariatric program and your desire/ability to utilize the offered support are probably more important than the type of procedure you choose.
- Gastric bypass surgery has been proven to be clinically useful for long-term weight loss. However, without the proper guidance before and after surgery, you may still fail.
Restrictive Vs. Malabsorptive
Weight loss surgery works because of restriction and sometimes malabsorption. Some surgical procedures involve only restrictive elements, while others include a combination of both.
Malabsorptive
Malabsorptive procedures alter the digestive tract so that a certain amount of the small intestine is bypassed. Bypassing the intestines allows for food to pass through the intestines quicker, resulting in fewer calories are absorbed.
Although some procedures are purely malabsorptive, none of these types of surgeries are performed for weight loss.
Restrictive
Restrictive procedures reduce the size of the stomach, so a patient feels full quicker. Restrictive surgeries most often use staples, and the stapled stomach is either removed or bypassed depending on the procedure.
Reducing the size of the stomach may also reduce ghrelin production and reduce hunger.
Restrictive procedures can be restrictive only or combined with a malabsorptive aspect.
The Procedures
For each procedure, we will provide the key benefits and risks and a link to learn more.
Remember to ask your doctor about his experience with each procedure. Have an open an honest discussion about your lifestyle to determine the best procedure for you.
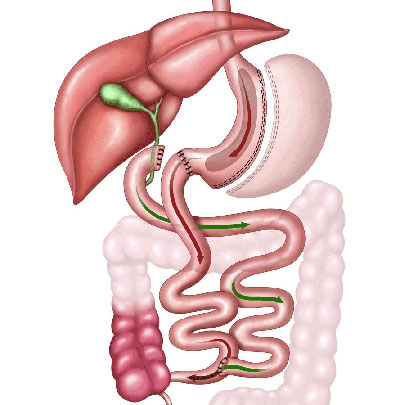
Gastric Bypass Surgery
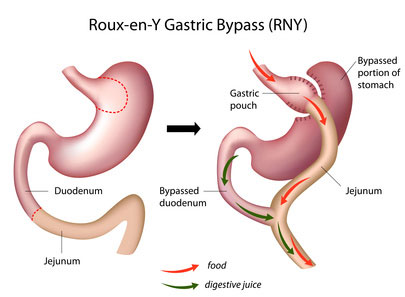 Average Excess Weight Loss: 60% to 80%
Average Excess Weight Loss: 60% to 80%
Serious Complication Rate: 1.25%
Average 30 Day Mortality Rate (Death Rate): 0.14%
Procedure Type: Restrictive and Malabsorptive
Key Benefits:
- A long history of success and clinical studies to validate its effectiveness.
- Average of 60% to 80% excess weight loss.
- May reduce hunger.
- Excellent rate of diabetes cessation after surgery.
- May relieve heartburn and acid reflux.
Key Disadvantages:
- It is a technically challenging procedure and typically requires a bit more time under anesthesia compared to other popular bariatric surgeries.
- Vitamins and minerals are required daily, or you’ll risk long-term nutritional deficiencies.
- If you are prone to ulcers, discuss this with your doctor.
Important Notes:
Gastric bypass restricts the amount you can eat and slightly reduces the amount of calorie absorption by re-routing your intestines. Some believe the re-routing of your intestines may produce a favorable change in gut hormones that increases satiety and reduces hunger.
Learn more about gastric bypass surgery.
Gastric Sleeve Surgery
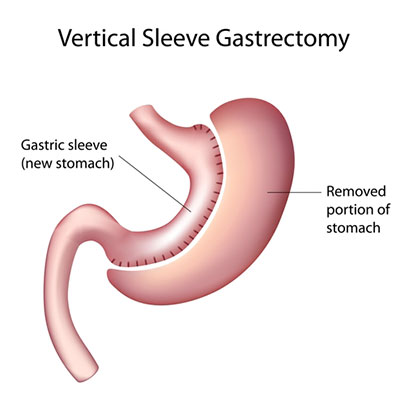 Average Excess Weight Loss: 57% to 70%
Average Excess Weight Loss: 57% to 70%
Serious Complication Rate: 0.96%
Average 30 Day Mortality Rate (Death Rate): .08%
Type of Procedure: Restrictive
Key Benefits:
- An average hospital stay of 2 nights, but in some cases, it is an outpatient procedure.
- Average of 60% to 70% excess weight loss.
- May reduce hunger.
- No foreign objects like Lap Bands.
- No re-routing of the intestines like gastric bypass.
- A straightforward procedure that is relatively easy to replicate.
Key Disadvantages:
- Vitamins and minerals are required for life. However, the risk of vitamin and mineral deficiencies is lower than the duodenal switch and gastric bypass.
- It does not improve heartburn or acid reflux and in some cases may worsen it.
- Less long-term data compared to gastric bypass.
Important Notes:
Re-routing your intestines is only a benefit if you prefer the least amount of anatomical change. Hunger reduction can be significant for some and not improve at all for others.
Learn more about gastric sleeve surgery.
Duodenal Switch Surgery
 Average Excess Weight Loss: 80% to 90%
Average Excess Weight Loss: 80% to 90%
Serious Complication Rate: 2% to 3%
Average Mortality Rate (Death Rate): 0.29% to 2.7%
Procedure Type: Restrictive and Malabsorptive
Key Benefits:
- The best weight loss profile, up to 85% excess weight loss.
- The best long-term weight loss success rate (better than 50% excess weight loss) of 95%.
- Best rate of comorbidity reduction.
Key Disadvantages:
- The highest risk for malnutrition.
- Strictest dietary guidelines.
- The longest and most complex procedure of the three primary bariatric procedures (bypass, sleeve, and duodenal switch).
- Highest 30-day serious complication rate.
- Strict adherence to vitamins and minerals and post-operative diet are required for success and to prevent malnutrition.
Important Notes:
Duodenal Switch surgery is not a new surgery. But because of it’s complexity and risk for malnutrition, many surgeons have shied away from the procedure. With better surgical tools, better support, and patient education teams, more clinical studies showing excellent success and reduction of comorbidities, and refinements to the procedure (i.e., SIPS – Stomach Intestinal Pylorus Sparing), the duodenal switch procedure is gaining in popularity.
It’s important to discuss this procedure with your surgeon. Your surgeon’s experience and his/her patient’s outcomes should be evaluated as well as their support program.
Learn more about duodenal switch surgery.

Gastric Balloons
Gastric Balloons are a new procedure for patients with a Body Mass Index (BMI) of 30 to 40 that want to lose weight but do not want to have surgery.
New options give the patient a pill to swallow, and a balloon is then inflated and left in the stomach for six months. Hunger is reduced, and satiety is increased.
These are not permanent. Lifestyle changes are paramount for lasting weight loss. Patients can expect 10 to 30% excess weight loss from gastric balloons.
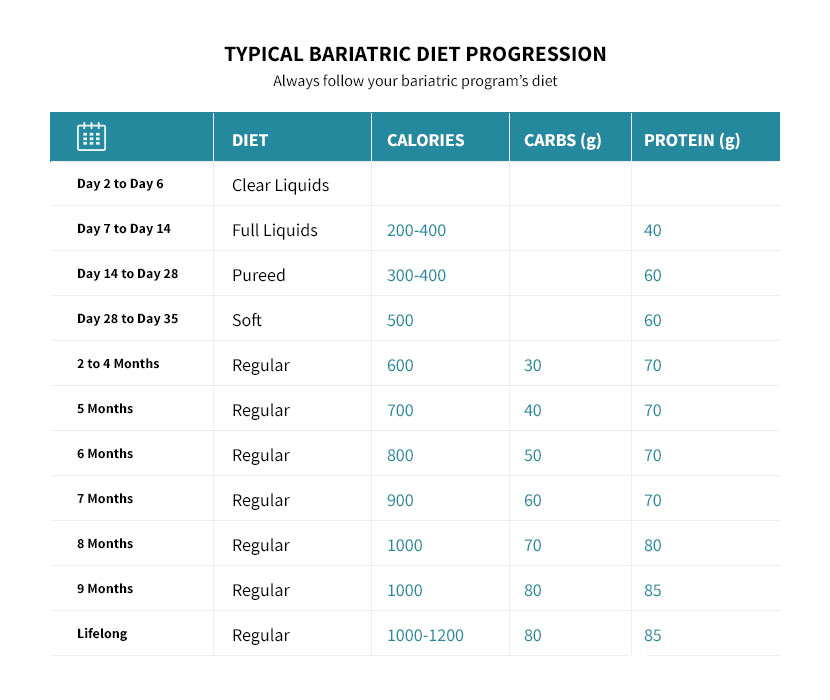
Your New Diet
Every bariatric program has slightly different diet guidelines. Different procedures may have different guidelines, as well.
The information below is not meant to replace your doctor’s or dietitian’s diet guidelines. It is, however, intended to give you an idea of what to expect with your new diet.
The Before Surgery Diet
Most bariatric programs recommend a one or two-week pre-op diet. The purpose of this diet is to reduce the size of your liver before surgery.
Many obese individuals have a fatty liver. Fat cells grow between liver cells and make the liver large, function poorly, and hard for your surgeon to move out of the way during surgery.
The pre-op diet is typically low in carbohydrates and high in protein. The diet forces your body to use your fat cells as energy. Your liver shrinks quickly, and surgery becomes safer and technically easier.
Low carb and high protein is typically recommended before surgery.
The After Surgery Diet
The typical post-operative bariatric surgery diet consists of four or five stages. Stages 3 and 4 are occasionally combined.
- Stage 1 – Clear Liquid Diet – For one or two weeks after surgery.
- Stage 2 – Full Liquid Diet – For one to two weeks after stage one.
- Stage 3 – Pureed Food – For one to four weeks after stage two.
- Stage 4 – Soft Foods – For one to two weeks after stage three.
- Stage 5 – Regular Diet – For the remainder of the patient’s life after stage three (starts typically 8 to 12 weeks after surgery).
Stage One – Clear Liquids
During the first stage, the patient’s diet will consist of water, broth, Jell-O, sugar-free popsicles, sugar-free crystal light. These substances should not contain any sugar or fat and should be consumed slowly.
You should avoid:
- Sugar
- Carbonated beverages
- Caffeine
Try your best to get 64 ounces of water. Dehydration is prevalent after bariatric surgery. Sip, sip, sip all day long.
The clear liquids let your stomach heal and prevent you from getting sick, which can also put undue pressure on your new stomach.
Stage Two – Full Liquid Diet With Protein
 Stage two typically focuses on liquids and protein. Below are common foods for stage two.
Stage two typically focuses on liquids and protein. Below are common foods for stage two.
- Non-fat Greek Yogurt
- Protein powder mixed with a sugar-free non-carbonated clear liquid.
- Protein powder mixed with Greek Yogurt.
- Protein shake in 4-ounce increments throughout the day.
- Sugar-free pudding.
- Soup with soft noodles.
- Non-fat yogurt.
- Carnation instant breakfast. Look for the sugar-free option.
- Very thin creamed soups. No chunks.
- Sugar-free sorbet.
- Very watery hot oatmeal. Check the sugar content.
- Sugar-free, nonfat ice cream
- Thinned applesauce. Check sugar content.
Staying hydrated is extremely important. Get your fluids in throughout the day by drinking 4 to 6 ounces every hour.
Stage Three – Pureed Foods
 Stage three typically focuses on introducing foods with a thin consistency. Below are some common foods for stage three.
Stage three typically focuses on introducing foods with a thin consistency. Below are some common foods for stage three.
- One protein shake per day.
- Almond milk or coconut milk makes a great protein shake.
- Hummus
- Cottage cheese (low fat)
- Soft cereals – Let your cereal sit in the non-fat milk until it’s soft.
- Soft vegetables – steam or boil them until they are soft.
- Soft cheeses – limit these, they are typically high in fat.
- Ground chicken or beef. Add some beef or chicken stock to keep the meat soft.
- Soups.
- Scrambled eggs – these are a great source of protein.
- Soft (steamed) fish. Remember to chew well.
- Canned tuna and salmon (you can add low-fat mayo) — a great source of protein.
- Mashed fruit. Bananas, avocados, and canned fruit (watch the sugar content).
You should avoid the following foods:
- While smoothies are ok, limit their sugar content. Most smoothies have a lot of sugar.
- Sugar
- Starchy foods like pasta, rice, and bread.
- Fibrous vegetables like celery, broccoli, asparagus, raw leafy green
500 calories is common at Stage 3. Remember to track with the Baritastic app!
Stage Four – Soft Foods
By this point, patients are typically excited to get back to more ‘normal’ foods. However, most programs still recommend choosing soft foods to prevent undue stress on your new stomach. Remember to follow your bariatric programs diet guidelines! Now is not the time to cheat.
- All foods from previous stages.
- Continue your daily protein shakes.
- Any fish.
- Chicken and other tender meats are typically allowed.
- Make sure you chew thoroughly and take small bites.
- Vegetables (it’s still recommended that you cook these to soften them a bit).
- Sweet Potatoes
- Healthy cereals
You should avoid the following foods in week four:
- Sodas
- Fried foods
- Fibrous vegetables (i.e., celery and asparagus)
- Sugary drinks
- Candy
- Dessert
- Pasta and other high carbohydrates, low nutrient foods (pizza).
- Whole milk and other whole milk dairy foods.
- Nuts
Stage 5 – Regular Diet
Its time to start your new life.
Admittedly, the hardest part and the most critical factor in your long-term success is your ability to implement a healthy, sustainable lifestyle. Does this mean you will never have a cookie again? Possibly, but probably not. It merely means you will choose healthy foods over unhealthy foods. You will shop healthy, and your body will receive its energy from nutrient-dense foods that keep you satiated.
You should choose healthy foods and have a good understanding of what is not healthy. For meals, protein is typically consumed first, followed by vegetables and finally by a small amount of healthy complex carbohydrates. Most programs recommend (recommendations vary based on target weight, height, and sex) the following macronutrient goals:
- ~1200 calories per day (this varies depending on the patient’s target weight and height)
- 65 to 85 grams of protein
- 40 to 80 grams of carbohydrates (ideally vegetables)
- Very little refined sugar
- Most programs don’t have patients monitor their fat intake as long as they are getting regular blood work. But choose lean meats whenever possible.
The Emotional Roller Coaster
Bariatric surgery produces drastic weight loss. As patients lose weight, hormones change. Obesity increases estrogen production in men and women (Reduced-Calorie Dietary Weight Loss, Exercise, and Sex Hormones in Postmenopausal Women: Randomized Controlled Trial). A rapid reduction in weight reduces estrogen. While losing weight at a fast rate in the months after surgery, patients often struggle to manage their emotions. The new restricted diet, along with the re-balancing of hormones, can produce irritability and emotional instability. For some patients, this is a minor inconvenience, others do not notice any emotional changes. But for some patients, the months after surgery can be difficult.
Self-perception, self-worth, and interpersonal relationships can change.
Acknowledging the potential for an emotional struggle and preparing for it can be helpful. The Emotional First Aid Kit is one of our top recommendations and worth a read for patients before or after bariatric surgery.
Does Insurance Cover Bariatric Surgery?
Insurance often covers bariatric surgery. While most of the major insurance carriers offer coverage for bariatric surgery, not all policies include coverage. To find out if your insurance policy provides coverage, we recommend three steps:
- Call your insurance carrier and ask if your policy covers sleeve gastrectomy surgery. Tell them to check CPT Code: 43775. Also ask if they cover CPT Code: 43644 (gastric bypass).
- It doesn’t matter which procedure you end up having. Calling your carrier is your first check to see if your policy includes coverage for bariatric surgery procedures.
- Call a local bariatric surgeon or bariatric program and ask if they’ll check if you have coverage.
- Most bariatric programs are happy to check and often have someone on staff that does this regularly.
- Use our bariatric program finder to find a bariatric program in your area.
- Familiarize yourself with your insurance companies requirements for coverage.
- Check your insurance company requirements for coverage here.
How Do I Get Started?
If you’re choosing to use insurance to cover the cost of bariatric surgery, it’s important to note that it takes about six months on average to get to surgery. Yep, it’s a long process. There are some benefits to this:
- Bariatric surgery is a tool to lose weight. If you don’t implement the necessary lifestyle changes, you risk weight regain, and the benefits of the surgery won’t be fully realized.
- The six months leading up to surgery help prepare you for life after surgery.
- During the six months leading to surgery, you will likely be required to undergo a psychological evaluation, a physician-supervised weight loss program, and possibly be required to lose weight.
- Fully engage in the process leading up to surgery and make sure you complete everything required by your insurance carrier.
Step 1:
The first step to get started is to find a bariatric program in your area and attend a seminar. Seminars, sometimes online, are a great way to learn more about the risks and benefits of bariatric surgery. I recommend attending an in-person seminar so you can meet the surgeon and or bariatric team. You may want to attend multiple seminars with different programs until you find a surgeon with whom you’re comfortable.
The second step is your initial consultation with the surgeon. The consultation is a one-on-one meeting with the surgeon where you’ll review your surgical options, discuss your lifestyle, and answer any questions you may have. You will likely leave with a piece of paper that outlines the necessary steps for approval. Many of these steps will be done outside of your surgeon’s office. Make sure you stay on track and set-up the needed appointments to get approval. Keep your surgeon’s office aware of your progress as you move through the checklist. We recommend using the checklist feature in the Baritastic app for this. Search the major app stores for Baritastic from your Smartphone (it’s free!).
The 10 Commandments for Bariatric Success
- You shall not consume foods that are primarily simple carbohydrates and lacking nutrients (i.e., chips, white bread, pasta).
- You shall walk and try to reach a goal of 10,000 daily steps.
- You shall eat protein, vegetables, and moderate amounts of fruits as your primary source of calories.
- You shall not drink your calories. You shall not drink soda.
- You shall take 20 seconds to chew each bite and be aware of the signs of fullness.
- You shall be prepared for emotional struggles and plan to overcome without ‘comfort foods.’
- You shall not gauge your success on a scale or your happiness on a number.
- You shall take your vitamins and minerals daily for the rest of your life to prevent devastating diseases.
- You shall have a support system — either friends, family, or online.
- You shall not eat food and drink fluids at the same time.
Conclusion
Bariatric surgery is a life-changing process. The surgery is a tool to help you lose weight. Once the weight comes off, it’s up to you to implement lifestyle changes that last. As you lose weight, exercise becomes more comfortable. The knowledge you’ve gained during your nutrition consults becomes invaluable. The friends you’ve made at support groups and the team of professionals at your bariatric program become indispensable.
So, which procedure is best for you? Whichever one you choose! It’s not the type of surgery you have, but rather your ability to stick to the guidelines and implement lifestyle change that lasts. All of the approved bariatric surgeries work.
Use your tool to take the hardest first few steps for you. Implement what you’ve learned, lean on the resources that you’ve gained. The next steps are up to you.