There are several things to consider when trying to decide between gastric bypass surgery and gastric sleeve surgery. Unlike the laparoscopic adjustable gastric band (Lap Band), these two operations are both permanent, reduce hunger, and lead to the highest percentage of weight loss. To properly compare gastric sleeve surgery to gastric bypass surgery we will examine the following data:
Amount of Weight Loss
It’s important to know how much weight you can expect to lose after surgery. It’s equally important to know that long-term weight loss is also dependent on your lifestyle and daily habits after surgery. Healthy exercise and eating habits (minimum 60 grams of protein per day, planned meals vs. grazing or unplanned snacking, etc.) will typically lead to more weight loss than the averages below.
If you do not implement healthy lifestyle changes after gastric bypass or gastric sleeve surgery, you may be more likely to gain a significant amount of weight back.
Gastric bypass patients lose between 60 to 80 percent of excess body weight in the first year. Gastric sleeve patients lose between 50 to 70 percent of excess body weight in two years.
The Averages
For individuals with a BMI over 45, gastric bypass is often recommended. Gastric bypass is preferred because it produces slightly more weight loss on average, and it creates ‘dumping syndrome.’
Weight loss for average person.
Because gastric bypass creates ‘dumping syndrome’ the patient is negatively reinforced with nausea, sweating, and a general ‘ill’ feeling shortly after they eat sweets, a large amount of carbohydrates, or high fat foods, like fried foods. This negative reinforcement can help reduce binging and limit high sugar and high fat food choices.
However, many surgeons are finding that gastric sleeve surgery is also very helpful with patients whose BMI is >45.
Gastric sleeve surgery removes 70% of the stomach where the hunger hormone ghrelin is produced.
This quickly and effectively reduces hunger and leads to excellent weight loss.
In fact, gastric sleeve surgery was originally created as the first step in a multi-stage procedure for people with a BMI over 50. Surgeons would create a sleeve and then finish the rest of the procedure (re-route intestines) after the patient had lost some weight. However, most patients lost enough weight from the first part of the procedure (the sleeve) that they didn’t need a second procedure.
Use this calculator to find out how much you will weigh after gastric sleeve surgery and gastric bypass surgery.
Regardless of which weight loss surgery you choose, you can expect to lose a certain amount of weight from bariatric surgery. This calculator will tell you how much weight you can expect to lose from each bariatric procedure and what you can expect to weigh two years after surgery.
The calculations are based on average weight loss per procedure. To lose the average amount of weight, you’ll need to follow your surgeon’s pre-operative and post-operative guidelines.
Long term diet and exercise changes along with other habit changes can lead to weight loss that exceeds the averages used in these calculations.
On average gastric bypass patients lose about 70% (Bariatric Surgery, A Systemic Review and Meta Analysis, 2004) of their excess weight. Gastric sleeve patients lose about 60% of their excess weight.
Comparison of Procedural Times
Going under anesthesia carries an inherent risk. The risk is higher for people that are considered obese. It’s even higher when you have co-morbidities like high-cholesterol and high blood pressure. While a minor factor in your overall decision, procedure time should be a factor in your decision.
By analyzing this information and adding it to the other factors involved, an individual will be able to make a more informed decision about which procedure might be better suited for their needs.
In an article from Obesity Surgery entitled “A Review of Laparoscopic Sleeve Gastrectomy for Morbid Obesity,” numerous studies were examined. The average procedural times for these two bariatric procedures were then calculated. The average length of time for the gastric bypass procedure was 2 hours and 44.8 minutes (164.8 minutes), and the average length of time for the gastric sleeve procedure was 1 hour and 40.4 minutes (100.4 minutes).
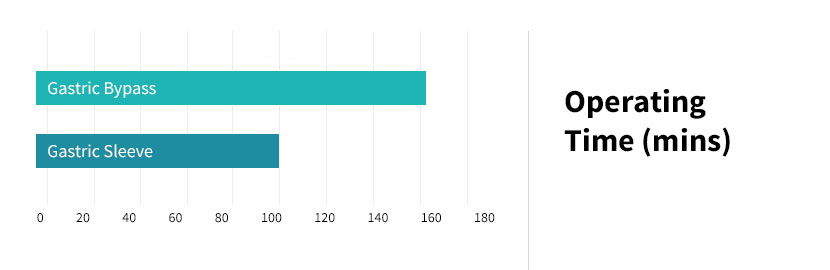
Chart showing operating times for gastric sleeve compared to gastric bypass.
Comparison of Weight Loss Speeds
As mentioned at the beginning of this article, weight loss is greater with gastric bypass surgery; however, by three years or more from the procedure date, the losses from gastric sleeve surgery begin to catch up with the losses from gastric bypass surgery.
In addition, the Body Mass Index (BMI) needs to be factored into the equation because this element of data will greatly affect the speed and amount of weight loss. The higher a patient’s IBMI (Initial Body Mass Index), the greater the drop of the patient’s BMI (especially after three years or more), regardless of procedure. Basically, the more body weight someone has prior to surgery, the faster they will lose body weight immediately after surgery.
WEIGHT LOSS SPEEDS
Gastric bypass produces almost all of its weight loss in the first year. Gastric sleeve surgery patients see weight loss continue through year two before they hit their target weight.
Losing weight quicker will get you to a healthier weight faster where it becomes easier to exercise and continue to implement healthy habits. However, losing weight over a two year period may reduce saggy skin and stretch marks.
Unique Benefits of Each Procedure
Both procedures are extremely safe and while one procedure takes more time (gastric bypass), this shouldn’t be your ‘aha’ factor when choosing your procedure.
Gastric bypass surgery is considered the ‘gold standard.’ That sounds good, right?
What’s The Benefit of Gastric Bypass Over Gastric Sleeve?
Many people will have different opinions on this question.
Why is gastric bypass considered the ‘Gold Standard’ and gastric sleeve surgery not?
- Gastric bypass surgery has been around longer. Its results and complications have been studied and its benefits proven. Every fellowship trained bariatric surgeon spent much of their training performing this procedure.
- Bypassing the intestines produces a malabsorptive aspect (less time for your body to absorb calories since your intestinal tract is shorter) that effectively reduces some calorie absorption.
- Gastric bypass is more complicated, has a slightly higher overall risk profile but it does produce more weight loss, and it creates dumping syndrome for most people.
- If you have a history of acid reflux (GERD), your surgeon may recommend gastric bypass instead of gastric sleeve surgery. There is a lower risk of GERD after gastric bypass.
Dumping syndrome sounds like a complication and a horrible side-effect of gastric bypass. It’s not. It’s a benefit. And it’s unique to gastric bypass surgery.
DUMPING SYNDROME
Also known as rapid gastric emptying, this condition occurs when too many sugary and/or fatty foods are consumed too quickly. The stomach then dumps the food material and gastric juices into the small intestine prematurely.
When an individual undergoes gastric bypass surgery, the pylorus is removed; this is the body’s safety valve that prevents the contents of the stomach from emptying into the small intestine too quickly. The body reacts by releasing gastrointestinal hormones in the small intestine and secreting insulin. Not everyone gets or experiences dumping syndrome. However, reports show about 80% of gastric bypass patients will experience dumping syndrome.
Early Dumping
There are two types of dumping syndrome: early and late dumping. The symptoms for early dumping usually occur 15 to 30 minutes after a meal and include nausea, diarrhea, cramps, bloating, dizziness, heart palpitations, sweating, and vomiting. You feel sick. Very sick.
Early dumping may occur if one eats foods that are either too cold or too hot; it can also be brought on by drinking liquids during a meal. The most common reason for early dumping is the consumption of sugary foods and large meals high in carbohydrates.
Late Dumping
Late dumping is a type of hypoglycemia (low blood sugar) and its symptoms usually occur about one to three hours after completing a meal. These symptoms include diarrhea, sweating, fatigue, weakness, dizziness, heart palpitations, fainting, and hunger. This condition may be controlled by consuming foods at a slower pace and by restricting one’s intake of sugary substances. Generally, the condition is controllable; however, it can become very serious if an individual continues to make dietary choices that lead to this. Including quality protein sources with every eating event is a way to help prevent dumping syndrome.
Why Dumping Syndrome is a Benefit
Remember Pavlov’s dog? His dog would salivate every time he saw his food. As he was testing how much the dog would salivate, he noticed that the dog started to salivate every time his researcher came into the room. The dog had begun to associate the researcher with his food and started to salivate when he saw the researcher.
Dumping syndrome is the Pavlov’s dog experiment with a negative reinforcement. Once you experience your first bout of dumping syndrome, your body is going to develop an extreme dislike of sugary, carbohydrate filled foods. At minimum your mind will warn you not to eat that donut or that piece of cake.
For people who have battled with obesity their entire life, this reminder and negative reinforcement helps curb consumption of less healthy foods.
Other Possible Reasons Why Bypass is the Gold Standard
Gastric Bypass is a complex operation performed by some of the most talented and highly trained laparoscopic surgeons. There is a level of pride in knowing how to perform this procedure. And not everyone can do it. It’s the most researched and studied weight loss surgery available. And it’s been around the longest and has thousands of success stories.
Benefits of Gastric Sleeve Over Gastric Bypass
Neither gastric bypass nor the sleeve is reversible. Both procedures offer a similar weight loss profile, albeit you’ll lose slightly more with gastric bypass.
Gastric sleeve surgery does offer some benefits over gastric bypass. The primary benefits are reduction of hunger and the speed and relative ease of the procedure.
The greater curvature (left side) of your stomach is thought to be the area where the hunger hormone ghrelin is produced. In gastric sleeve surgery this area is removed almost entirely. The result is significantly reduced hunger. Some patients report having to remind themselves to eat for the first 6 months after surgery.
It’s important to note that with gastric bypass you do have a smaller pouch (stomach) and ghrelin production is also reduced. However, there is some data that seems to indicate less hunger with gastric sleeve surgery post-operatively compared to gastric bypass.
- Another purported benefit of gastric sleeve surgery is a slower weight loss profile. Typically, gastric sleeve patients see their weight loss plateau after 2 years while gastric bypass produces much quicker weight loss (typically all within the first year).
Risk of Complications
The risk associated with each procedure needs to be looked at as well. This includes complications that might occur immediately after surgery or several months later. Some of these complications are minor and some can be serious.
However, mortality (the risk of death) is not a major issue with either surgery. This is especially true with laparoscopic cases. While open procedures have a higher mortality rate, it is still below one percent.
Complications of Gastric Bypass Surgery
For severe complications call 911 emergency.
Complications can and do happen.
Below is an overview of the common complications associated with gastric bypass. They are listed in order of least serious to most serious.
NAUSEA
Nausea is another common side effect of gastric bypass surgery. Following the doctor’s and/or nutritionist’s recommendations for dietary intake usually improves this condition. In addition, receiving a larger amount of IV fluids at a faster rate also assists with improving these complications. The average risk of nausea is 70%.
DEHYDRATION
Dehydration is a depletion of fluids and is very common after gastric bypass surgery; however, it is usually managed if the patient drinks enough water in the weeks following the surgical procedure. Two liters a day is usually the amount of water that is recommended. Not consuming enough water may cause vomiting, which could lead to worse dehydration and other complications. If the dehydration is severe enough, an individual may have to receive more IV fluids. An individual’s risk for dehydration may be as high as 65% or more. Stay hydrated by sipping at least 8 oz. of fluid every hour, for 8 hours each day.
INDIGESTION
Dyspepsia (indigestion) can be defined as difficulty with digesting food; this condition is accompanied with a burning sensation or discomfort in the upper abdomen. Treatment consists of changing one’s diet by avoiding greasy foods. It may also be treated by only drinking liquids for a certain amount of time. Antacids and H2 blockers are used to treat this condition if dietary changes do not work. A patient’s risk for indigestion is usually somewhere around 60% or more.
REACTIVE HYPOGLYCEMIA
This situation occurs when a patient has low blood sugar. It generally occurs 45 to 60 minutes after eating a meal high in carbohydrates. Symptoms may include lightheadedness, increased heart rate, and sweatiness. This is because there is an imbalance between blood sugar and insulin within the bloodstream. Insulin allows sugar to be processed, but if the insulin remains in the blood after the sugar from the meal has been used, then it causes low blood sugar. Consuming a few ounces of diluted juice or two ounces of skim milk has proven to be effective treatment for this condition. To prevent reactive hypoglycemia, an individual should avoid sugar and eat proteins first.
As a complication of gastric bypass surgery, hypoglycemia often occurs because of excessive dumping after the surgery. Medications will usually manage conditions; however, surgical removal of a portion of the pancreas may be required in more extreme situations. The risk for this condition is around one percent.
NUTRITIONAL DEFICIENCIES
Nutrition deficiencies are very common both before and after surgery, regardless of the procedure type. These deficiencies include osteoporosis, anemia, and metabolic bone disease. These deficiencies may be prevented with appropriate vitamin and mineral supplementation, including a bariatric specific multivitamin every day and calcium citrate.
GALLSTONES
Individuals who have gastric bypass surgery have a 33% chance of developing this condition. Gallstones are formed from pieces of cholesterol and other matter inside the gallbladder and/or bile passages. The possibility of getting gallstones increases dramatically when an individual experiences extreme weight loss. Prevention of gallstones may be achieved with bile salts, or by making sure you consume some healthy fats each day like olive oil, avocado, or nuts and seeds.
INCISIONAL HERNIA
This dangerous condition involves the intestine becoming obstructed. A hernia is an opening that occurs when an internal organ or body part protrudes through a surgical incision; it occurs inside the abdomen or through the abdominal wall muscles. An internal hernia may result from surgery and rearrangement of the bowel. An incisional hernia is an incision that does not heal in a correct manner. Abdominal wall hernia is more likely to occur with open procedures than with laparoscopic procedures and usually occurs several months after surgery. Although the rate of this condition can be as high as 20% with open surgery patients, laparoscopic patients have a risk of only 0.2%.
WOUND INFECTION
Incisions may be infected because of bacteria released from the bowel during the operation. This may also happen to the inside of the abdomen; however, bladder and kidney infections may also occur. Antibiotics, respiratory therapy, and physical activity after surgery can lower these risks. These types of infections are far more common with open surgery than with laparoscopic techniques. The average rate for developing this risk is 12%.
MARGINAL ULCERS
Marginal ulcers are the most common in the newly created stomach pouch after gastric bypass surgery. They can usually be avoided by following the correct dietary guidelines. They may also be avoided by not smoking and not using NSAIDs (including ibuprofen). These ulcers are often accompanied by a burning pain in the stomach, and their presence can be confirmed with an endoscopy (a scope inserted into the mouth and down the esophagus). They are usually treated with antacids. Gastric bypass patients have a 12% chance of developing ulcers.
STOMAL STENOSIS (STRICTURE)
A stricture is when a constriction of the opening to or from the stomach becomes inflamed and/or blocked, preventing food from properly entering the stomach or intestines. Although this condition occurs with gastric sleeve surgery, it is most common in gastric bypass surgery and results from a build-up of scar tissue. Strictures can be either acute or chronic (very quick onset or an ongoing issue after surgery). Symptoms include food intolerance, dysphagia, nausea, and vomiting. Strictures found immediately after surgery may be treated with bowel rest (not consuming food by mouth) and rehydration with intravenous fluids. These strictures will usually heal, and if they do not, then endoscopic dilation is performed in order to restore the opening. The risk of this complication is 8%.
ANASTOMOTIC LEAKS
This condition occurs when a connection made during surgery leaks digestive contents into the abdomen. This situation may produce infections and can often be fixed if it is found quickly enough. By blowing air into the connection and using a dye, a surgeon can see if the connection is secure. The risk for leaks is 5%.
HEMORRHAGE
Common symptoms of postoperative bleeding include hematemesis (vomiting of blood) or melena stools (bloody stools). There are two types of hemorrhages: intraluminal and extraluminal. Intraluminal bleeding is often managed by using large bore intravenous lines for fluid resuscitation, administration of packed red blood cells, measurement of urine with a Foley catheter, and performing an urgent gastroscopy. Common sources for extraluminal bleeding include the gastric staple line, spleen, liver or abdominal wall. Urgent laparoscopy allows for the evacuation of the clot and control of the bleeding source. Hemorrhages can also be treated by replenishing bodily fluids, discontinuing the use of anticoagulation drugs, and by transfusion or operation. The risk of hemorrhage after gastric bypass surgery is 3.2%.
VENOUS THROMBOEMBOLISM
The coagulation of the blood is increased whenever the body is injured or undergoes a surgical procedure. Sometimes, a clot in the veins of the leg will form, break free, and then float to the lungs. This type of clot is called a pulmonary embolus, and it can be life threatening. It should also be realized that there is an increased possibility of this occurrence if the patient’s body does not move much after the procedure. In order to combat this problem, blood thinners are administered immediately before the surgical procedure is to begin. The risk of deep vein thrombosis or pulmonary embolism is around one percent.
Complications of Gastric Sleeve Surgery
You’ll notice the complications for gastric sleeve surgery are very similar to gastric bypass. For a thorough explanation of gastric sleeve complications, this article is recommended.
GASTROESOPHAGEAL REFLUX DISEASE
Gastroesophageal reflux disease (GERD) is a long-term complication that is very common with gastric sleeve patients. It is characterized by periodic episodes of gastroesophageal reflux and usually accompanied by heartburn. It often leads to histopathologic changes, which are microscopic structural changes in the esophagus. It may also lead to esophagitis, which is an inflammation of the esophagus.
It is usually treated with proton pump inhibitors. If symptoms persist, a gastroscopy (which is an examination of the esophagus, stomach, and duodenum using an endoscope) is performed. The risk for GERD can be as high as 47%.
NUTRITIONAL DEFICIENCES
Like gastric bypass surgery, complications relating to malnutrition are also possible. This is especially true if the recommended nutrient supplementations are not taken.
STRICTURE (CHRONIC)
Chronic strictures generally require endoscopic or surgical treatments. Treatment options depend on the length of narrowed portion. If the narrowing is short, endoscopic dilatation is used. However, if the narrowing is long and endoscopic dilation fails, then surgery is often necessary. Some patients have even required a gastric bypass in order to alleviate this condition.
GALLSTONES
Gallstones are also developed in individuals who have gastric sleeve surgery. This is because the overall chance of getting them increases whenever anyone experiences an enormous amount of weight loss. In the same manner as patients who have had gastric bypass surgery, prevention of gallstones is usually achieved with bile salts. The risk for this complication can be as high as 23%.
STRICTURE (Acute)
This condition most commonly occurs with gastric bypass surgery; however, it is sometimes seen in patients who have undergone gastric sleeve surgery. Like strictures found in gastric bypass patients, treatment is accomplished by not consuming food orally and by rehydration with IV fluids. Endoscopic dilation is also performed occasionally on gastric sleeve patients with this condition. The risk for stricture (including chronic stricture) is 3.5%.
VENOUS THROMBOEMBOLISM
Although the risk of this condition is much greater for gastric bypass patients, it occurs to a lesser degree with gastric sleeve patients. The risk of deep vein thrombosis or pulmonary embolism with gastric sleeve patients is below one percent.
STAPLE LINE FAILURE
One of the more immediate concerns of gastric sleeve surgery, this aspect of the procedure is given special attention by surgeons, who spend a lot of extra time and effort in order to make sure that the newly created barrier performs correctly. When the staple line does fail, the patient will often experience an increase in heart rate. Other symptoms include breathing problems and/or an increase in body temperature. If the leak occurs a few days after surgery, laparoscopy may be attempted in order to find and repair the leak. However, if the leak begins a week or more after the operation, then the area is drained and then either treated with stents or washed out depending upon the stability of the patient. The overall risk for this condition (including delayed failure) is 2.4%.
Other Considerations

EXPERIENCE LEVEL OF YOUR SURGEON
The average learning curve of a surgeon is generally 100 surgeries or more. Because of this factor, the experience of a surgeon should be carefully considered. In addition, many surgeons will have more experience with one procedure than the other, and this element should also be taken into consideration. This article discusses how to choose your surgeon.
Gastric Bypass is a complex operation performed by some of the most talented and highly trained laparoscopic surgeons. There is a level of pride in knowing how to perform this procedure. And not everyone can do it. Keep this in mind when asking for your surgeon’s opinion on which procedure is right.
Ask him how many gastric bypass procedures he has performed and how many sleeve procedures. Understand that gastric sleeve has only become commonplace in the last 5 years and most insurance companies did not include coverage for this procedure until 2011.
PERSONAL OPINION OF YOUR SURGEON
An experienced surgeon should review your medical information as well as your lifestyle.
It often takes a third party to notice habits that you may not be aware you’ve created. Certain habits, like severe binge or emotional eating are difficult to stop. Gastric bypass may be more appropriate for you. Your surgeon has seen many patients and has records of their success and failures. Because of these unique insights your surgeon’s opinion should not be discounted
Have an open an honest discussion with your surgeon about your fears and your goals. You should walk away confident that you chose the best procedure for you.